Market Trends of Global Revenue Cycle Management Industry
The Claims and Denial Management Segment is Expected to Witness Significant Growth Over the Forecast Period
Claims and denial management involves reviewing the denial procedure. Solution providers of denial and appeal management are involved in reviewing patient documentation and resubmitting the claim.
Hospitals and medical care facilities that do not have an expert team depend on third-party solution providers. Companies with a good understanding and experience of insurers' provider guidelines revert to insurers with explanations and requests for payment. Sometimes, the denials may be reversed by a telephone conversation with the insurer, followed by a written appeal, focusing on why the claim cannot be denied. Denial management services help regulate the financial stability of healthcare settings and improve patient satisfaction by streamlining the Medical Billing process during hospital admissions.
Hospital revenue is declining with more healthcare facilities under intense scrutiny and a rise in healthcare claims. Thus, such issues are expected to raise the adoption of Revenue Cycle Management solutions by healthcare providers for maintaining hospital revenues and boost the segment's growth. For instance, in September 2023, Cigna Group paid USD 172 million to resolve False Claim Act allegations. It was stated that the company had submitted and failed to withdraw inaccurate and false diagnosis codes for the Medicare Plan Advantage enrollees to boost its payments from Medicare. In August 2023, the US Department of Labor sued the United Health Group for denying thousands of patients payments for emergency room services and urinary drug screenings. Therefore, healthcare providers are expected to utilize RCM solutions to regulate the financial stability of healthcare facilities, contributing to the segment's growth.
Strategic initiatives taken by key players are also expected to boost their capabilities in developing Revenue Cycle Management Software, thus contributing to the segment's growth. For instance, in February 2023, Experian Information Solutions Inc. launched a new AI-driven product, AI Advantage, which provides real-time intelligence and predictive modeling to resolve the issues associated with the high volume of healthcare insurance denials and help healthcare providers recover billions of dollars lost in insurance claim denials. Thus, new services for claims and denial management launched by companies are likely to be adopted by healthcare providers, propelling the segment's growth over the forecast period.
Factors such as the need for claims and denial management services in hospitals due to their significant advantages and the new service launches are anticipated to contribute to the market's growth over the forecast period.
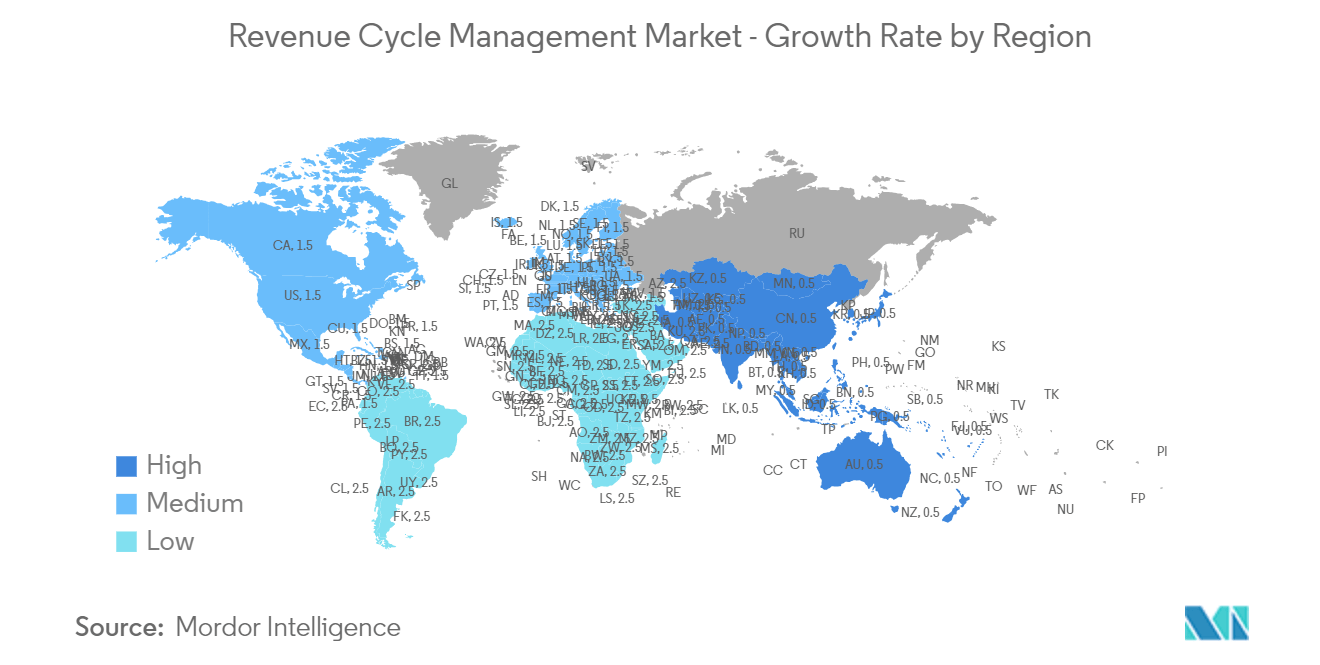
North America is Expected to Hold a Significant Share of the Revenue Cycle Management Market
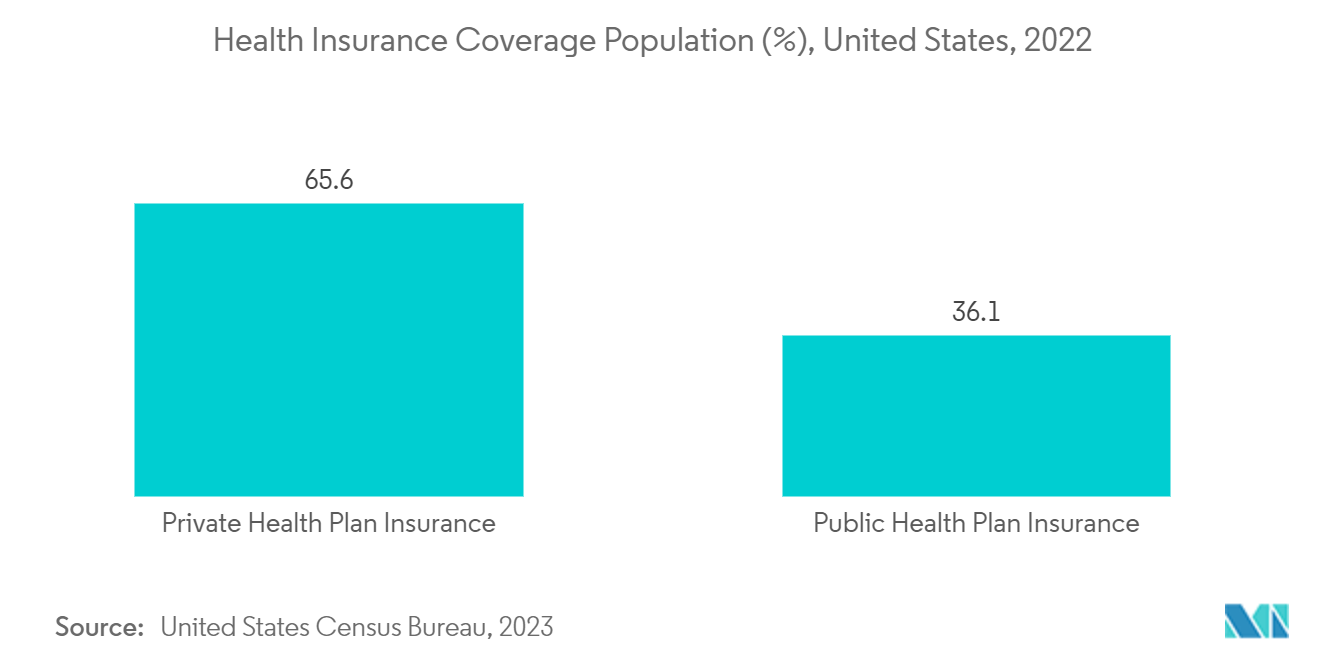
North America's Revenue Cycle Management Market is anticipated to grow significantly over the forecast period due to substantial regulatory changes affecting the finances, organization, and delivery of healthcare services.
Government initiatives are likely to improve the development of Healthcare Revenue Cycle Management solutions, thus driving the regional market's growth. For instance, in December 2023, the Healthcare Financial Management Association and Xsolis, an AI technology company, introduced the Executive Revenue Integrity Council in the United States to address revenue cycle and reimbursement concerns through networking and education.
Most healthcare providers in the region are deploying Revenue Cycle Management (RCM) systems that reduce the time to receive payment after providing a service. The RCM systems facilitate various tasks associated with Medical Billing with automation and help save time. Thus, they are likely to be adopted by healthcare providers in hospitals, which may drive the market's growth in the region.
A large amount of patient data generation and increasing healthcare burden may lead to errors in Medical Billing and other processes, which may further propel the demand for Revenue Cycle Management solutions over the forecast period. For instance, in May 2023, according to the Consumer Protection Bureau, the prevalence of Medical Billing Errors in the United States was estimated at around 7-49%, thus increasing the demand for revenue cycle management.
The key players are adopting various strategies, such as acquisitions, collaborations, partnerships, and expansions, to increase their market shares and contribute to the market's growth. For instance, in September 2022, AGS Health launched the AGS AI Platform. This connected solution blends artificial intelligence (AI) and automation with award-winning human-in-the-loop services and expert support to maximize revenue cycle performance in the United States. In May 2022, Cerner Corporation partnered with AKASA to use artificial intelligence (AI), a driven platform for automating eligibility checks, denials, and claims processing, to boost revenue cycle workflow automation.
Thus, factors such as government initiatives, the increasing need to reduce medical billing errors, and new service launches are expected to drive the market in North America during the forecast period.